Autistic disorders, Attention-Deficit Hyperactivity Disorder (ADHD), and common childhood disorders are all accelerating exponentially in the 21st century. It is time to stand back and ask what is the underlining problem and solution.
Clinically the eight year old was diagnosed with sensory integration disorder. His mother believed there was more to her son’s challenges than this, however. Her son’s teacher aide suggested that she come and visit us at the Therapeutic Centre.
Sensory Processing Disorder (SPD, also known as Sensory Integration Dysfunction) is a controversial condition that exists when multisensory integration is not adequately processed in order to provide appropriate responses to the demands of the environment.
Sensory processing problems are usually identified in children. But they can also affect adults. Sensory processing problems are commonly seen in developmental conditions such as autism spectrum disorders.
Research, observation and the careful study of the case history of individuals with ASDs reveals they often have major disruptions in the gut, brain and immune (GBI) axis. Over the last few decades there have been numerous publications explaining how nutrigenomics plays an integral part in determining the outcome of a child’s development and expression of pre-disposed genes to different health exposures down the generation. Other factors contributing to ASDs are dysbiosis, leaky gut, impaired detoxification and environmental toxins, all of which can interfere with the healthy functioning of each system in the GBI axis, predisposing a child to ill health, and ultimately leading to the destruction of the microbiome terrain in the gut.
We considered all the above factors before developing a customised protocol for our client.
Case History
An eight year old caucasian boy presented at our clinic with the following challenges:
- Subject was born three weeks prematurely.
- Subject had a forceps birth, resulting in a hæmatoma on his head.
- At three years old he developed asthma and was placed on Flextidine and Ventolin.
- Mucous nasal passage.
- Numerous digestive problems, resulting in hospitalization. Stomach cramps.
- Late vaccination, including tetanus. Travelled a lot.
- Had one dose of MMR vaccination. Afterwards had severe rash so course of vaccinations was discontinued.
- Medically diagnosed with Sensory Intergration issues.
- Had behavioural issues from age of four years old.
- Difficulty interacting with peers especially in larger settings.
- Constantly disrupted concetration.
- Subject struggled with reading.
- Subject likes strong flavours. He craves oily things e.g. he can eat whole can of anchovies.
- Subject very fidegety, unsettled and restless.
- Subject didn’t like to be touched.
Treatment
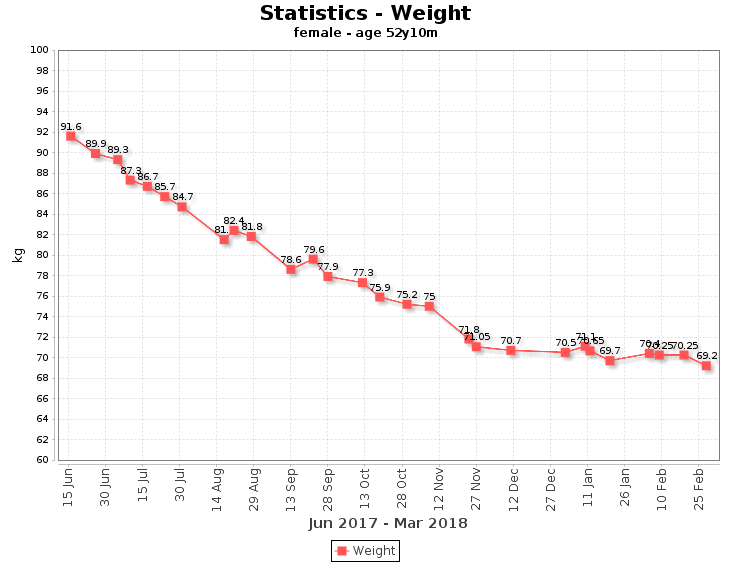
We developed a protocol to detox the cellular matrix, enabling the gut to respond positively. Subsequently the nervous system behaviour pattern becomes aligned to the signalling of the brain. We used the TC Smart Practice Management System to monitor and track progress, and provide live data visualisation support enabling responsive and lightning-fast decision-making as new data arrived.
| Recommendation | Dose | Rationale |
|---|---|---|
| Glyconutrients | 1 tsp twice daily | Improve concentration and cellular communication |
| Children’s Lipid Complex for Brain Support | 1 tsp daily | Supply fat soluble nutrients for brain structure and function |
| Children’s Gut, Liver and Detoxification Support | 2 scoops twice daily | To reduce toxicity and heavy metal accumulation |
| Children’s Multivitamin and Mineral | 1 tsp daily | Provide essential nutrients |
| Children’s Stress and Anxiety Relief | 1 tsp daily | If presenting with hyperactivity |
| Healthy Blood Glucose Support | 1-2 tablet daily | Glucose regulation |
| D-Lactate Free Probiotic | 1 capsule twice per day | To support the gut microbiome |
- Elimination of all processed food, gluten, dairy, wheat, and sugar.
- Introduction of more green vegetables, organic chicken, lean meat, and fish.
- One fruit a day
- Increasing the intake of water
Educating the mother and ensuring her comprehension of the protocol formed a huge part of the successful outcome.
Net Outcomes
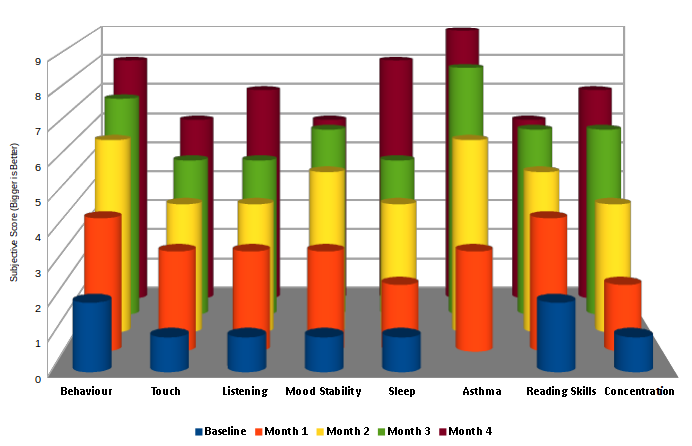
| Month | Changes Noticed |
|---|---|
| Month 1 | Major improvement in Asthma Nasal mucus and phlegm significantly reduced Bowel motion twice daily Night toilet visits reduced School attendance more regular |
| Month 2 | Good at taking all supplements Singing and dancing in a school play, and coping well Better focus We noticed he was quieter, sitting patiently at the reception (and keen to drink a herbal tea) Noticeable change to cuddles. Now likes a cuddle. |
| Month 3 | Asthma under control Getting good reports from school Even more focussed. Additional learning support one hour for literacy and maths. Now sleeping on his own bed. Breathing is much better. No longer constantly clearing his nose and throat. Food intake now balanced. He is eating well and not craving for sweets. |
| Month 4 | Sleeping on his bed 3 – 4 nights of the week No symptoms of Asthma. Previously with cold weather like this year, he needed inhaler support. He hardly takes the preventer either. He is happy and now likes going to school. Doing well there. Reads picture books. Much less absenteeism from school. Now asking lots of questions and wanting to know about his flight overseas. Interested in things. Well occupied in school. |
Conclusion
This case demonstrated that in addition to working on the GBI axis, it is of paramount importance to work with and expect co-operation from the family concerned to achieve results in a short time.
Constant dialogue, encouragement and tracking of the progress itself provide the confidence and belief that possibilities can be created for the child’s future.